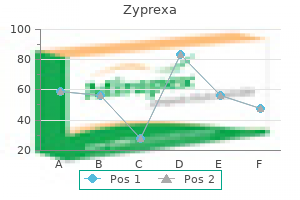
Order zyprexa with a visa
Eslicarbazepine acetate: start treatment at 400mg od (tablets will need to be split) symptoms brain tumor zyprexa 7.5mg on-line. Oxcarbazepine (all indications): start treatment at 300mg bd; increase weekly in steps of up to 600mg to a maximum dose of 2. Liver and renal function should be assessed 6- to 12-monthly throughout treatment. Pharmacokinetics and interactions Pharmacokinetics Oxcarbazepine and eslicarbazepine acetate are both prodrugs which are converted to eslicarbazepine in the liver. Peak plasma concentrations are reached at different time points, depending on the formulations used: conventional tablets at 712h, chewable tablet at 76h, and liquid at 72h. Due to reduced bioavailability, a 125mg suppository is equivalent to a 100mg oral tablet. Carbamazepine is metabolized by the liver into a number of derivatives, including the pharmacologically active carbamazepine-10,11-epoxide. Eslicarbazepine acetate: eslicarbazepine acetate is a prodrug, rapidly converted by hepatic first-pass metabolism to the active metabolite eslicarbazepine. Eslicarbazepine acetate Levels decreased: carbamazepine, phenytoin, and topiramate 3. Eslicarbazepine acetate Levels decreased: lamotrigine, topiramate, valproate, and warfarin Levels increased: phenytoin 3. Oxcarbazepine Levels decreased: carbamazepine, felodipine, lamotrigine, levetiracetam, rufinamide, and topiramate Levels increased: phenobarbital and phenytoin Pharmacodynamic interactions 1. Oxcarbazepine With lithium and lamotrigine: enhanced neurotoxicity As a result of the magnitude of the interaction between carbamazepine and ketoconazole and between carbamazepine and quetiapine whereby ketoconazole and quetiapine plasma levels are decreased to almost non-detectable values, these drug combinations can be considered contraindicated. Oxcarbazepine placebo-controlled, dose-ranging trial in refractory partial epilepsy. A meta-analysis of individual patient responses to lamotrigine or carbamazepine monotherapy. Levetiracetam, oxcarbazepine, remacemide and zonisamide for drug resistant localisation-related epilepsy: a systematic review. The latter is used secondline due to the rare, but significant, risk of severe liver dysfunction. Gastrointestinal: abdominal pain, constipation, diarrhoea, dry mouth, dyspepsia, gastritis, nausea, taste disturbance, and vomiting. Monitor closely in cases of mild to moderate hepatic impairment, although no dose alteration is routinely recommended. Thirteen per cent of patients did not complete the study, due to withdrawal of consent and adverse events. There is no evidence that use early in the disease course prevents or delays motor complications. Levodopa dose often needs to be reduced by approximately one-third, or the dosing interval may need to be extended. It is the active metabolite of prednisone (itself inactive) and is used for long-term disease suppression. Methylprednisolone and prednisolone: the uses of methylprednisolone and prednisolone are very broad. This leads to modulation of leucocyte activation, migration, cytokine production, and overall suppression of humoral responses. Toxicity and side effects Short courses of steroids are typically associated with minor and transient side effects. These include dyspepsia, sleep disturbance, mood changes, confusion, infection risk, and impaired glucose tolerance. Musculoskeletal: avascular necrosis of the hip is an important, but rare, potential side effect, which can occur after a single course. Dexamethasone has a lower propensity to cause psychosis but is more likely to cause steroid myopathy and weakness due to its fluorinated chemical composition. In addition, side effects, including osteoporosis, hypertension, hypokalaemia, diabetes, skin thinning, and infection, may be more severe in the elderly. These patients require frequent monitoring for complications, and lower dosing may be necessary. Although doses of <40mg/day are unlikely to cause systemic effects in the infant, it is recommended that adjustments are made to the dosing interval to allow 4h before breastfeeding. Methylprednisolone and prednisolone are used to treat a large number of autoimmune and inflammatory conditions. For a discussion of the evidence base for its use in these indications, see the individual conditions. It does not affect overall mortality, but subgroup analysis has shown that it reduces mortality in meningitis caused by S. It is associated with an increase in recurrent fever, but not in other adverse events. Nonetheless, up to 75% of patients treated with dexamethasone show neurological improvement at 48h, and practical guidelines provide low-level recommendations of use, based on symptom severity. Dexamethasone should be withdrawn as rapidly as feasible, although in some patients with widespread cerebral oedema or particularly aggressive tumours, a slower taper may be required. The general principles are that prednisolone can be started at high doses of 1mg/kg od, but a maximum dose of 60mg is recommended for most conditions. Such high doses can be used in the longer term in some conditions but are usually tapered after the first week or month. This typically involves dose reductions of 10mg/week, until a daily dose of 30mg is reached. This taper may need to be titrated to symptoms, and slower decrements of 1mg/month may be initially needed in certain conditions such as neurosarcoidosis. Monitoring Patients should be monitored for the development of common side effects noted above, with provisions made to reduce the total steroid dose as soon as possible with steroid-sparing anti-inflammatory medications. In patients on high-dose steroids, consideration should be given to the co-prescription of medications for bone and gastric protection. Mechanism of action the predominant mechanism of action for this group of drugs is through activation of post-synaptic dopamine receptors to restore nigrostriatal dopaminergic output. Bromocriptine and cabergoline are long-acting agonists selective for D2 receptors, having no significant affinity at D1 receptors. Gastrointestinal: abdominal pain, constipation, diarrhoea, dry mouth, nausea, and vomiting.
Purchase 5mg zyprexa free shipping
The association of medical comorbidity in schizophrenia with poor physical and mental health medicine lodge ks buy 10mg zyprexa mastercard. Clozapine use and relapses of substance use disorder among patients with co-occurring schizophrenia and substance use disorders. Alcohol use disorders in schizophrenia: a national cohort study of 2,653 patients. The impact of substance use disorders on the course of schizophrenia-a 5-year follow-up study: dual diagnosis over 5 years. Prevalence of alcohol use disorders in schizophrenia: a systematic review and meta-analysis. Rate of cannabis use disorders in clinical samples of patients with schizophrenia: a meta-analysis. Serious mental illness and tobacco addiction: a model program to address this common but neglected issue. Interventions for smoking cessation and reduction in individuals with schizophrenia. A randomized, double-blind, placebo-controlled study evaluating the safety and efficacy of varenicline for smoking cessation in patients with schizophrenia or schizoaffective disorder. Does varenicline worsen psychiatric symptoms in patients with schizophrenia or schizoaffective disorder A placebo-controlled trial of bupropion combined with nicotine patch for smoking cessation in schizophrenia. Smoking in patients receiving psychotropic medications: a pharmacokinetic perspective. Lifetime positive symptoms in patients with schizophrenia and cannabis abuse are partially explained by co-morbid addiction. Cannabis-induced psychosis and subsequent schizophrenia-spectrum disorders: follow-up study of 535 incident cases. Cannabis use and risk of psychotic or affective mental health outcomes: A systematic review. Cognitive impairment in dual diagnosis inpatients with schizophrenia and alcohol use disorder. Naltrexone and disulfiram in patients with alcohol dependence and comorbid psychiatric disorders. Psychotic spectrum disorders and alcohol abuse: a review of pharmacotherapeutic strategies and a report on the effectiveness of naltrexone and disulfiram. Effects of acamprosate on cognition in a treatment study of patients with schizophrenia spectrum disorders and comorbid alcohol dependence. Psychosocial treatments for people with co-occurring severe mental illnesses and substance use disorders (dual diagnosis): a review of empirical evidence. A pilot study comparing motivational interviewing and an educational intervention in patients with schizophrenia and alcohol use disorders. Psychosocial interventions for the long-term management of patients with severe mental illness and co-occurring substance use disorder. Randomized controlled trial of motivational interviewing, cognitive behavior therapy, and family intervention for patients with comorbid schizophrenia and substance use disorders. Feasibility of a skills training approach to reduce substance dependence among individuals with schizophrenia. A randomized clinical trial of a new behavioral treatment for drug abuse in people with severe and persistent mental illness. Randomized controlled trial of contingency management for stimulant use in community mental health patients with serious mental illness. Chapter 7 Special Populations Children and the Elderly Children with Schizophrenia the diagnostic criteria for childhood-onset schizophrenia is the same as is used for adult-onset schizophrenia, and the disease process is considered to be the same. However, those who develop schizophrenia as children will likely experience a more severe form of the disorder as they grow into adulthood. These children who are diagnosed with schizophrenia are approximately twice as likely to have a parent with a psychotic-spectrum disorder than those who develop schizophrenia as adults (5). Also, 25% of those determined to have childhood schizophrenia were at one point given an autism-spectrum diagnosis (6). The prodromal phase of childhood schizophrenia is marked by diminished school performance, poor impulse control, increased aggression and hostility, and bizarre behaviors, including altered eating and hygiene habits (7, 8). Auditory hallucinations have been the most reported positive symptom, and these are simple rather than conversational or commenting voices. Delusions are the next most commonly reported symptom and often incorporate childhood material. Childhood and adolescent-onset disease clinically present very similarly, but the timing of onset can vary markedly; childhood disease is characterized as being more insidious rather than acute, perhaps contributing to underdiagnosis and delayed treatment (3). Differential Diagnosis Psychotic symptoms have been reported by nearly 0% of children without mental illness. These are most often experienced as hallucinations and delusions and occur without the concurrent bizarre behavior or deterioration in functioning seen in those with mental illness (4). A number of other primary childhood psychiatric disorders can share symptoms of schizophrenia. The most common differential diagnoses include the childhood anxiety disorders, including obsessive-compulsive and 77 77 Schizophrenia 78 post-traumatic stress disorders, and mood disorders of depression and bipolar disorder, as well as pervasive developmental disorders. Increased alertness and startle reactions may be prominent, which are also unusual in schizophrenia. Depression While children with depression can experience associated psychotic features of hallucinations and delusions, unlike those with schizophrenia, children with psychotic depression usually do not demonstrate significantly disorganized speech or behaviors. A family history of bipolar disorder is also helpful in pointing toward an affective disorder. Personality Disorders Schizoid personality traits in children include solitariness, unusual fantasies, excessive interest in unusual topics, increased sensitivity, and paranoid ideas and an unusual style of communication; continuation of schizoid personality disorder into adolescence and adult life is most often reported (24). Schizotypal personality disorder is characterized by marked abnormalities in social and interpersonal behavior, cognitive and perceptual distortions, and transient psychotic-like symptoms. The most common clinical outcome for children with schizotypal personality traits is development of this disorder. Treatment Appropriate treatment involves both psychopharmacological as well as psychosocial interventions. Antipsychotic medications are effective for reducing psychotic symptoms and preventing recurrences. However, other first- and second-generation antipsychotics are also likely to be effective. The earlier and more effective the treatment, the better the long-term outcome related to symptom control, as well as connection with the mental health care system. Antipsychotics provide effective symptom control, and of these, risperidone and clozapine have been most widely studied. Similar-but often more severe-side effects are seen with children as with adults. Risk factors for the development of these include higher doses, longer duration, female sex, and prenatal complications. Similar to adults, it is important to monitor liver dysfunction, weight gain, hyperprolactinemia, hyperglycemia, and hyperlipidemia in children. Children and adolescents have a higher liability to experience antipsychotic-induced hyperprolactinaemia, weight gain, and associated metabolic disturbances than adults. Olanzapine is associated with the highest weight gain and is considered as a second-line antipsychotic for children and adolescents (35). Psychosocial treatments include strong familial support when available, education for caretakers, behavioral modifications, psychotherapy, academic modifications, and assistance and enhancement of social and cognitive skills. Elderly Patients with Schizophrenia the number of patients aged 55 and older with schizophrenia is expected to increase substantially during the coming decades (36).
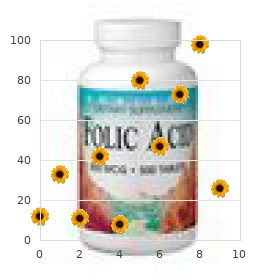
| Comparative prices of Zyprexa | ||
| # | Retailer | Average price |
| 1 | Brinker International | 417 |
| 2 | Office Depot | 502 |
| 3 | Verizon Wireless | 697 |
| 4 | Alimentation Couche-Tard | 752 |
| 5 | Kroger | 209 |
| 6 | SUPERVALU | 475 |
| 7 | Trader Joe's | 231 |
| 8 | Staples | 992 |
| 9 | Safeway | 778 |
Order cheap zyprexa on line
They are also more likely to have pharmacokinetic interactions with other co-prescribed medications and are more commonly predisposed to side effects medications versed order cheap zyprexa on line, including sedation and reduced nutritional intake, and hence lower dosing regimens are often appropriate. If the medication is continued, then highstrength folic acid should be given throughout pregnancy. Valproate levels decrease markedly during pregnancy; hence, if treatment is to be continued, rises in the dose may be required. If valproate treatment is continued during breastfeeding, then infants should be monitored for adverse effects, including haematological effects, and, if these are identified, the infant should be switched to an alternative feeding regimen. It found clear evidence that valproate was more effective than lamotrigine and more tolerable than topiramate, and hence should be considered first-line in the treatment of generalized epilepsy. In contrast, a multicentre, double-blind trial carried out in 1992 comparing the efficacy of valproate with carbamazepine in focal-onset epilepsy demonstrated that carbamazepine gave better long-term control of seizures and had fewer side effects than valproate. Pharmacokinetics and interactions Pharmacokinetics oral bioavailability is >90% for standard-release medications. Valproate is 90% bound to plasma proteins (less in the elderly due to reduced albumin levels). Valproate undergoes extensive hepatic metabolism to multiple metabolites via the cytochrome P450 enzyme system. Valproic acid glucuronide and 3-oxo-valproic acid constitute just over one-third of these metabolites each. Some of the minor metabolites are pharmacologically active at a similar level to valproate. More than 97% of valproate is renally excreted, the majority as metabolites and 73% as unchanged drug. Valproic acid is effective in migraine porphylaxis at low serum levels: a prospective open-label study. Valproate (valproic acid or sodium valproate or a combination of the two) for the prophylaxis of episodic migraine in adults. A comparison of valproate with carbamazepine for the treatment of complex partial seizures and secondarily generalized tonic-clonic seizures in adults. It is given in far higher doses than for cardiovascular indications, and so patients are at particular risk of bradycardia and heart block. Mechanism of action Verapamil is a calcium channel blocker and has been shown to block Ptype calcium channels in the rat striatum. Verapamil may exert its predominant effect by inhibiting calcium channels in the hypothalamus, i. In severe hepatic impairment, verapamil should be reduced to one-third of the normal dose, and titration should be done carefully, with close monitoring of the heart rate and rhythm. Careful monitoring should also be undertaken in renal impairment, as there are limited data on verapamil toxicity in renal disease. There are no reported cases of teratogenicity associated with verapamil use in humans. Efficacy In a double-blind, randomized, placebo-controlled trial of 30 patients with cluster headache, 12 of the 15 patients on verapamil experienced a >50% reduction in headache frequency after taking verapamil for 2 weeks. Half of these experienced a reduction in headache frequency within the first week of treatment, while, at the end of 2 weeks, four patients in the verapamil group were headache-free. The dose of verapamil used was 120mg tds, and side effects were minimal, with no test subject discontinuing treatment due to side effects. Verapamil in the prophylaxis of episodic cluster headache: a double-blind study versus placebo. It is a narrowspectrum drug, predominantly used in the treatment of infantile spasms. Its main limitation to be used as a broader-spectrum agent in epilepsy is its high incidence of visual field defects. In addition, it is licensed as a monotherapy for the treatment of infantile spasms in children aged 1 month to 2 years old. Neurological: dizziness, fatigue, headache, impaired attention and memory, paraesthesiae, speech disorder, and tremor. Ophthalmological: visual field defects have been reported in up to a third of patients. The defects are typically a concentric constriction in both eyes, more prominent nasally than temporally. These defects occur months to years following initiation of treatment and may be dose- and length of treatment-dependent. It may be as a result of an idiosyncratic drug reaction or an accumulation of vigabatrin in the retina. Subsequent optic neuritis and atrophy have been reported, and it is recommended that vigabatrin is discontinued when field defects are detected. Psychiatric: aggression, agitation, depression, excitation, nervousness, and paranoia. Caution should be taken if other retinotoxic drugs are prescribed and if there is a prior history of behavioural problems, depression, or psychosis. No information is available on pharmacokinetic changes of vigabatrin during pregnancy. No studies have been performed to assess the level of vigabatrin in breastfed infants. If used, infants should be monitored for potential side effects, and, if these are identified, the infant should be switched to an alternative feeding regimen. Efficacy As an adjunct in focal-onset epilepsy, with or without secondary generalization, the proportion of patients experiencing a 50% or more reduction in seizure frequency was 48% vs 26% for placebo in one double-blind, placebo-controlled trial. Therapeutic drug monitoring Measurement of plasma levels may be useful in ascertaining compliance where doses of between 1 and 3g/day would be expected to have plasma levels of 0. Vigabatrin as add-on therapy for adult complex partial seizures: a double-blind, placebo-controlled multicentre study. Prevalence of visual field loss following exposure to vigabatrin therapy: a systematic review. It was first licensed for use in the 1960s, initially in the treatment of leukaemia, although its indications have subsequently expanded. Its myelosuppressive effects are relatively mild, compared to other chemotherapeutic agents. Mechanism of action Vincristine inhibits neoplastic cell proliferation by binding to tubulin, thus preventing microtubule formation and stopping cell cycling during metaphase.
Purchase cheap zyprexa on line
These are more likely during the first dose symptoms blood clot leg discount zyprexa 7.5 mg fast delivery, with high infusion rates and with long delays since the last dose. If side effects occur, the infusion should be stopped, and the patient appropriately treated. Depending on the nature of the side effect, the infusion can be recommenced at a lower rate and increased as tolerated. Immunoglobulins and their complexes are mostly broken down by the reticuloendothelial system. Evidence-based guideline: intravenous immunoglobulin in the treatment of neuromuscular disorders: report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. This is available as a solution at a concentration of 5mg/mL in 4mL, 20mL, and 40mL vials. Avoid in those with hepatic impairment, as severe hepatocellular injury has been reported. However, labetalol should be used in caution with hepatic impairment, as hepatocellular injury can occur, and labetalol is predominantly eliminated in the urine; hence dose adjustment may be required in renal impairment. The primary outcome assessed was mortality or dependency at 14 days post-symptom onset; this occurred in 61% of patients who were actively managed, and 59% of patients treated with placebo (rr 1. Importantly, at 3 months post-stroke, the rates of mortality were halved in those who were actively treated (Hr 0. Pharmacokinetics and interactions Pharmacokinetics Labetalol binds to plasma proteins (90%) and is extensively metabolized in the liver to produce inactive glucuronide metabolites, excreted in the urine (50%) and bile. Its main advantage is its paucity of pharmacokinetic interactions, and its main disadvantage is a high incidence of gastrointestinal side effects. Mechanism of action the precise mechanism of action of lacosamide is poorly understood. In vitro studies have shown that the compound selectively enhances slow inactivation of voltage-gated sodium channels, thereby stabilizing neuronal membranes. Fatigue, impaired concentration and memory, insomnia, tremor, and nystagmus are common. It is recommended to use lacosamide with caution in severe hepatic impairment, although there is a lack of clinical data in this population. Animal studies have demonstrated teratogenic effects; however, there are no studies in humans. If lacosamide is taken during breastfeeding, infants should be monitored for side effects, and an alternative feeding regimen used if these are identified. Efficacy the efficacy of lacosamide has mainly been explored in the context of refractory epilepsy. Dosing and monitoring Dosing For the treatment of epilepsy, start treatment at 50mg bd. This can be increased by 50mg bd in weekly intervals to a recommended maximum dosage of 200mg bd. Routine monitoring Liver and renal function testing should be performed prior to commencing therapy and then yearly while treatment is ongoing. Forty per cent is excreted unchanged by the kidneys, with the majority of the hepatically metabolized product. Adjunctive lacosamide for partial-onset seizures: efficacy and safety results from a randomized controlled trial. It may be slightly less effective than carbamazepine in the treatment of focal-onset seizures but benefits from having fewer side effects. It typically occurs in the first 8 weeks or if medication is suddenly stopped and resumed. An antihistamine or a topical corticosteroid can be started, and the patient should be monitored closely for the development of new symptoms/ spread of the rash. This risk is increased with: younger patients, concomitant use of valproate, rapid initiation of medication, and atopic individuals. It is now thought that the risk of serious skin rash is comparable to other medications, such as carbamazepine and phenytoin, which have traditionally been seen as safer. The rash may also rarely represent the beginning of a multiorgan hypersensitivity syndrome. Gastrointestinal: hepatic failure is very rare and usually, but not always, occurs within the context of a hypersensitivity reaction. Haematological: rarely, blood dyscrasias can occur, including anaemia, leucopenia, pancytopenia, and thrombocytopenia. The dose should be reduced in hepatic dysfunction-50% of the dose should be used in moderate hepatic impairment, and 25% in severe hepatic impairment. Metabolites may also accumulate in renal failure; hence the maintenance dose should be reduced in severe renal impairment. Lamotrigine plasma concentrations will decrease markedly during pregnancy by up to two-thirds; hence an increase in dose may be required. Infants should be monitored for potential side effects, such as fatigue and irritability, and an alternative feeding regimen used if these are identified. The results suggested that lamotrigine and carbamazepine may have similar efficacy for focal-onset seizures, but that lamotrigine is more likely to be tolerated by patients. Valproate was found to be more effective than lamotrigine for generalized seizures. Dosing and monitoring Dosing As a rule, uptitration of lamotrigine is performed slowly to reduce the incidence of side effects. If oral dosing is stopped for >5 days, then slow uptitration will need to be restarted. Routine monitoring Hepatic and renal function should be assessed prior to starting and yearly while treatment is ongoing. Lamotrigine also undergoes autoinduction, so that clearance may increase by up to 37%, requiring an increase in dose. The half-life for lamotrigine varies dramatically, depending on whether valproate or enzyme-inducers are co-prescribed. It is very effective, and has simple pharmacokinetics and a relatively good side effect profile.
2.5mg zyprexa sale
It uses the optical property that the absorption of near-infrared light is dependent on the amount of oxygenated and deoxygenated haemoglobin present in the tissue (Owen-Reece et al medicine cups discount zyprexa generic. Source and detector pairs can be placed on the surface of the skull and local changes in the intensity of the emitted and absorbed light can quantify changes in tissue oxygenation. In addition, absolute parameters such as blood flow and cerebral blood volume can be calculated. The measurement of changes in haemodynamic activity-as a proxy measure of functional brain activity-is based on the assumption that increased tissue oxygenation represents an increase in regional cerebral blood flow, associated with an increase in underlying neural activity (Logothetis et al. Recently, this technique has been used in neonatal studies investigating cerebral responses following noxious stimulation. Cortical haemodynamic activity has been recorded in infants in response to noxious events, including heel lance, venepuncture, and endotracheal tube suctioning and repositioning (Bartocci et al. The technique provides an opportunity to record the electrical activity generated by large populations of cerebral neurons. By recording from multiple electrode sites, it is possible to obtain a representation of the spatial distribution of the electric field recorded over the scalp. In addition, an increase in characterized rhythmical patterns of activity, such as delta brushes and temporal sawtooth waveforms, is observed, followed by their subsequent disappearance (Dreyfus-Brisac and Monod, 1972). From the subplate grows the thalamo-cortical and cortico-cortical connections (Kostovic and Rakic, 1990), with its neurons contributing to the first evoked potentials from 24 weeks of gestation (Hrbek et al. Highly sensitive assessment of grey and white matter and the differentiation of myelination in white matter can be visualized. In vivo, the transient subplate zone can be seen as an area of hypointensity on magnetic resonance images (Prayer et al. This could be extrapolated to other neonatal conditions, possibly including the assessment of pain. However, even asleep, infants show distinct brain activations to cognitive (Redcay et al. Assuming that the cortical hubs denote areas involved in tasks requiring high information processing (Sporns et al. These evoked patterns of activity are referred to as evoked or event-related potentials. By considering the features of the evoked activity, such as the polarity, timing, and topography, inference can be made about the how the brain processes noxious sensory information. An event-locking technique has been developed to enable the evoked neuronal activity following a single clinical noxious event to be recorded (Fabrizi et al. Use of this technique has provided electrophysiological evidence that the immature infant brain can discriminate between acute noxious and non-noxious stimulation from 35 gestational weeks (Slater et al. These electrophysiological measures of nociceptive-specific brain activity are useful for understanding how the developing human brain responds to nociceptive stimuli, and may potentially be useful to test the ability of analgesic treatments in neonates to suppress these increases in brain activity. Nevertheless, these experimental studies are challenging and require specialist data acquisition and analysis skills (Fabrizi et al. There appears to be a gradual shift with advancing maturity, from non-specific bursts of neuronal activity to modality-specific activity that is discriminative between noxious and non-noxious events. In contrast, there is no difference in the magnitude of the evoked response following non-noxious simulation. Although it cannot be concluded that prior pain experience specifically alters the subsequent processing of nociceptive information, it is clear that some aspect of being born preterm differentially alters the cerebral response to nociceptive stimuli compared with non-noxious tactile stimuli. It is possible that the anatomical alterations observed in infants exposed to excessive nociceptive inputs may underpin some of the functional differences in subsequent nociceptive processing. Nevertheless, direct measurement of brain activity may further our understanding of how noxious events are processed by the infant nervous system. Brain regions, which classically form part of the adult pain matrix, were activated during noxious stimulation but were not observed during non-painful warmth stimulation. Further, ex-preterm children displayed an increased sensitization to painful stimuli without habituation. A recent imaging development may begin to disclose the reorganization of cortical hubs. With resting-state functional connectivity being based, but not exclusively, on direct anatomical connections (Damoiseaux and Greicius, 2009), the assessment of the functional and structural relationships in the infant brain may begin to be investigated. Randomised trial of fentanyl anaesthesia in preterm babies undergoing surgery: effects on the stress response. The cutaneous withdrawal reflex in human neonates: sensitization, receptive fields, and the effects of contralateral stimulation. A comparison of the mechanically and electrically evoked flexion reflex as a quantifiable measure of responses to innocuous and noxious skin stimulation in human neonates. The cutaneous flexion reflex in human neonates: a quantitative study of threshold and stimulus/ response characteristics, following single and repeated stimuli. Beyond feeling: chronic pain hurts the brain, disrupting the default-mode network dynamics. Visual functional magnetic resonance imaging in patients with Sturge-Weber syndrome. Greater than the sum of the parts: a review of studies combining structural and resting-state functional connectivity. Conclusion the measurement of evoked brain activity in response to nociceptive stimuli in preterm and term born infants may help validate existing behavioural, somatic motor, and autonomic measures of nociception. In addition, these techniques may help in the development of more robust clinical tools for measuring infant pain. This brain-oriented approach to understanding nociception must be considered alongside the existing body of literature that characterizes the clearly observable neonatal behavioural and physiological responses to noxious stimulation. It would be ideal to develop a specific neural biomarker that is a direct correlate of pain experience, however, in the absence of language this is out of our grasp. Influence of repeated painful procedures on prefrontal cortical pain responses in newborns. Advances in magnetic resonance neuroimaging techniques in the evaluation of neonatal encephalopathy. Functional neuroimaging of speech perception during a pivotal period in language acquisition. Flexion reflex of the limb, crossed extension reflex, and reflex stepping and standing. Latency to facial expression change following noxious stimulation in infants is dependent on postmenstrual age. Brain mapping in sedated infants and young children with passive-functional magnetic resonance imaging. Cutaneous hypersensitivity following peripheral tissue damage in newborn infants and its reversal with topical anaesthesia. The postnatal development of the cutaneous flexor reflex: comparative study of preterm infants and newborn rat pups. Spontaneous fluctuations in brain activity observed with functional magnetic resonance imaging. Development of visual and somatosensory evoked responses in pre-term newborn infants. C-Fos can be induced in the neonatal rat spinal cord by both noxious and innocuous peripheral stimulation. Postnatal changes in responses of rat dorsal horn cells to afferent stimulation: a fibre induced sensitisation. Correlation between the sequential ingrowth of afferents and transient patterns of cortical lamination in preterm infants. A new interpretation of the laminar development of the cerebral cortex: synaptogenesis in different layers of neopallium in the human fetus. Developmental history of the transient subplate zone in the visual and somatosensory cortex of the macaque monkey and human brain.
Syndromes
- Obesity
- Fatigue or overexertion
- Liver problems, such as hepatitis B or hepatitis C, cirrhosis, liver failure, and autoimmune and alcoholic hepatitis
- Infertility
- Bluish-colored fingernails and lips
- Shortness of breath
- Other serious illnesses, such as heart disease, liver cirrhosis, or diabetes mellitus
- Infection (a slight risk any time the skin is broken)
- Keeping your skin clean and moist and avoiding your specific psoriasis triggers may help reduce the nubmer of flare-ups.
- Cystic Fibrosis Foundation - www.cff.org
Order cheapest zyprexa and zyprexa
Behavioural strategies include skills such as relaxation treatment chlamydia purchase 10 mg zyprexa otc, exposure and desensitization, and modelling. Children are also taught behavioural strategies to relieve physiological discomfort and relearn adaptive functioning patterns. Treatment focuses on modifying this negative belief, enhancing ability to solve pain-related problems, and providing a set of skills for managing pain in an adaptive way. It is typically delivered individually in weekly therapy sessions, though it can also be effectively administered in a group format (Barakat et al. Although the literature has not yet clearly identified which constellation of cognitive or behavioural interventions are most effective for specific groups based on characteristics such as age, gender, or type of pain, there is strong evidence that taken as a whole, these strategies are highly effective for treatment of acute and chronic pain for children as well as adults (Eccleston et al. For example, a child with a chronic pain condition such as complex regional pain syndrome would be taught that she would not cause harm to herself by using her affected limb. A child preparing for a painful procedure would be taught that pain sensations are diminished when attention is allocated away from painful stimuli. Both developmental level and individual child coping style may influence utility of these techniques. Psychoeducation for chronic pain For chronic pain, psychoeducation entails providing the child and family with a clear explanation of what chronic pain is. Psychoeducation should include a rationale for how and why cognitive-behavioural strategies can effectively reduce pain and restore function. It is helpful to incorporate written educational materials so that children and families can refer back to them as needed. A meta-analysis of this evidence shows positive effects of preparation on observer reports of pain during needle procedures but insufficient evidence of effects on self-report of pain or behavioural measures of distress (Uman et al. Psychoeducation for paediatric chronic pain is rarely delivered as a stand-alone intervention; thus, there is little literature examining its effectiveness in isolation. Educational interventions provide a rationale for how and why other cognitive-behavioural strategies can effectively reduce pain and distress. Preparation for procedural pain Preparation is a specific educational intervention that entails explaining to the child in advance exactly what the procedure will involve. Typically this includes breaking down the procedure into detailed steps to reduce anxiety and uncertainty. Preparation can include showing the child where the procedure will occur and specific equipment that will be used. Recent theories, backed by empirical support, hold that distraction can exert a powerful analgesic effect that alters the activity on pain processing pathways in the brain (Bantick et al. Distraction can include both behaviourally oriented strategies such as blowing bubbles or playing a videogame, and cognitively oriented strategies such as non-procedure focused conversation or tasks. Reading stories or watching videos are also effective distractions for many children. Distraction for procedural pain Distraction is perhaps the most commonly employed cognitivebehavioural technique for coping with procedural pain. It is easily employed in this setting and can work well across a variety of ages and temperaments. Distraction techniques are generally not time intensive, require little advance preparation, and can be implemented by a variety of clinicians. Often, children benefit most from education strategies that require them to assume a more active role. Therefore, rehearsal, in which the child him/herself acts out the procedure, such as through medical play, can reduce anxiety and foster positive coping. Often, assuming the role of the doctor or nurse and performing the procedure on a stuffed animal or parent helps children acquire a sense of mastery of an anxiety-provoking situation that may otherwise feel uncontrollable. In general, studies support preparation and modelling/rehearsal strategies as effective tools for reducing anxiety and distress about medical procedures (Harbeck-Weber and McKee, 1995) with some indication that they may help reduce pain as well. Children and adolescents can identify activities that they enjoy and find absorbing and can be encouraged to use those activities in attempts to cope with pain. School can also be framed as an adaptive distraction from pain, since children are more likely able to distract themselves from pain in school than when home in bed, for example. It is important to work with the individual child to identify the distractions that work best. Evidence base for distraction Among all the specific cognitive behavioural tools for managing procedural pain, distraction has the largest base of empirical support (Cohen et al. Cognitive reframing can take place prior to , during, and after a painful procedure. Using cognitive reframing after a procedure, sometimes referred to as memory alteration, is aimed at reducing the negative memories of a painful experience so they are not as distressing and do not predispose the child toward greater anxiety in subsequent painful procedures (Chen et al. Modelling and rehearsal Modelling and rehearsal techniques are aimed at reducing anticipatory anxiety by helping the child to develop more realistic expectations of a potentially painful situation and increasing comfort and familiarity with the situation. Once recurrent negative thoughts are identified, the therapist and child examine evidence supporting the thought. Current evidence suggests that graded in vivo exposure effectively reduces pain and fear-avoidance beliefs and behaviours. The intervention led to greater reductions in pain, disability, pain-related discomfort, and fear of pain compared to standard multidisciplinary treatment (including medication) for children with chronic pain. However, this small study has not been replicated, so results should be interpreted cautiously. The overall pattern of findings did not meet criteria to be considered efficacious in a metaanalysis (Uman et al. Relaxation techniques: breathing, guided imagery, muscle relaxation Relaxation strategies focus on acquiring specific skills that can be used to decrease pain perception by promoting a general sense of physical and psychological well-being. The roots of this approach lie in classical conditioning theory, which holds that the association between the stimulus. Typically, systematic desensitization entails developing a hierarchy of anxiety-provoking situations ordered from least- to most-feared. Through a process called graded in vivo exposure, the child is then exposed to the fearful situations beginning with those identified as least feared and gradually working up the hierarchy. The goal is to encounter the situations safely, without the previously experienced distress, to unlink them from associated anxiety. Relaxation techniques in procedural pain In the brief context of procedural pain experiences, deep breathing is perhaps the most commonly used relaxation tool. Often props such as bubbles or party blowers are employed, particularly with younger children; these tools incorporate a component of distraction that can augment the benefits of deep breathing. Recorded instructions for progressive muscle relaxation and guided imagery procedures are available and can be used in procedural settings when there is less preparation time available. Relaxation techniques for chronic pain Relaxation is widely used in chronic pain. Learning to employ relaxation strategies in a self-directed manner provides children a greater sense of control over their physiological processes, which may help counteract feelings of helplessness induced by chronic pain. Sometimes these techniques are taught using computer-based biofeedback (see Zeltzer, Chapter 60, this volume), providing concrete visual and/or audio feedback to help the child gain increased awareness over previously involuntary physiological processes. Many therapists provide children with audio-recordings to practise techniques between sessions. In addition to using guided imagery to develop relaxing images, this technique can also focus on pain-reducing imagery. These techniques are typically more effective when the child has been guided into a general state of relaxation prior to engaging in imagery exercises (Kuttner, 1991). Desensitization in procedural pain Desensitization is a time-intensive strategy that requires a number of sessions with a trained clinician prior to the procedure. Therefore, in the procedural pain context it is typically used with children who are known to have high levels of pain-related anxiety in response to medical procedures such as injections. Desensitization in chronic pain Expectancy effects have a strong influence on pain perception. Many children with chronic pain develop a pattern of avoiding activities they believe will trigger or increase pain (Martin et al. Desensitization can be used to reduce this pain-avoidance pattern, unlink the association between activities and fear of pain, and help children to re-engage in activities, which can in turn help to reduce pain.
Buy generic zyprexa on line
However medications for factor 8 cheap zyprexa 10mg without a prescription, a lack of randomized controlled trials in children means that evidence from adult studies guides pharmacological management of neuropathic pain in children, which is problematic as the aetiologies and mechanisms are different. In this article we propose an algorithm for drug therapy for neuropathic pain in children based on best available evidence, our clinical experience, and the safety of these drugs in paediatric practice. We suggest a step-wise approach incorporating first-, second-, third-, and fourth-line therapies that should be tried methodically according to effectiveness and side effects. Neuropathic pain in children, if identified and treated in a timely manner as part of an interdisciplinary framework, using multimodal strategies can be managed effectively. Though it is well known that children suffer from neuropathic pain, there have been few paediatric studies. Moreover, it is likely that given the differences in nervous system anatomy and physiology between adults and children, as well as different aetiologies of neuropathic pain, there are significant differences in mechanisms and prognoses. Though basic mechanisms underlying pain transmission are reasonably well understood, neuropathic pain is a complex, interdependent dynamic state, which is likely influenced by multiple factors including aetiology, previous pain experience, and genetic factors. Interindividual variability in chronic pain expression and response to analgesics are known to have a genetic basis, which may guide future treatments (Sorge et al. Translation of these mechanisms into drug therapy has not been simple, further complicated by the fact that underlying mechanisms in children are different from those in adults. Examples include the increased plasticity of the developing nervous system and altered response to injury, and the reduced spinal microglial response to nerve injury during earlier stages of development (Moss et al. One could postulate that these differences might improve the prognosis of neuropathic pain in children. Nociceptive pain is initiated by normal activation of pain pathways by noxious stimuli, whereas neuropathic pain is associated with abnormal activation of pain pathways involving both the peripheral and central nervous system. It is a complex, Clinical features Neuropathic pain is characterized by positive symptoms and negative symptoms (sensory loss, numbness). Positive symptoms may be understood in terms of pathological changes in the peripheral nerves, as a way in which the nervous system attempts to compensate for sensory loss. A high index of suspicion is required to make a diagnosis of neuropathic pain, and an early clue is the poor response to simple analgesics such as acetaminophen and non-steroidal antiinflammatory drugs. Common pain descriptors include burning, throbbing, electrical, stabbing, shooting, pricking, and pins and needles. In addition to positive and negative symptoms, autonomic dysfunction can sometimes be seen. Neuropathic pain: children versus adult Neuropathic pain in adults affects up to 8% of the population with significant impact on quality of life (Torrance et al. This might in part be due to a lack of an agreed definition and diagnostic criteria for paediatric neuropathic pain. In addition, compared to adults, the common causes of neuropathic pain in adults are rare in children. Moreover, most of the adult literature from which paediatric neuropathic pain management is extrapolated is based on common adult aetiologies. With clearer diagnostic instruments for paediatric neuropathic pain, and improved recognition and understanding, it is likely that the prevalence in children is more than we would like to think. Neuropathic pain is often part of a mixed picture alongside nociceptive pain, for example, vaso-occlusive pain in sickle cell disease (Niscola et al. Drugs the drugs used in the symptomatic management of neuropathic pain in children are presented in a step-wise, practical manner, based on our clinical experience in paediatric practice, the implications of committing children to certain therapies, and best quality evidence (Levels 1 and 2). The evidence comes from adult studies as very few clinical trials have been conducted in children with neuropathic pain, and the literature is predominantly case series or isolated case reports. With inadequate or partial pain relief, additional drugs can be added in combination (with exceptions noted in the text-see Table 48. The multimodal mechanism of action comprises blockade of serotonin and noradrenaline reuptake, interaction with sodium and calcium ion channels, as well as some antihistamine and anticholinergic antagonism. Additional benefit may not be seen beyond 2400 mg/day Decrease by same rate if unhelpful. Topical Lidocaine 5% patch Each plaster or patch is applied over intact, dry and non-irritated skin for a period of 12 h on and 12 h off. After 2 weeks convert total daily dose to long-acting preparation and keep short-acting preparation for breakthrough. No ceiling effect; dose escalation can proceed with careful titration, but at high daily doses (180 mg), efficacy should be re-assessed and opioid switch or alternative options considered. Topical lidocaine 5% medicated plasters provide an alternative pharmacological non-systemic option in the treatment of neuropathic pain with good evidence in adults supporting its use in herpetic neuralgia (Binder et al. Lidocaine plasters are also effective in combination with other antineuropathic analgesics and reduction in co-analgesic consumption was demonstrated in a retrospective observational study in adults. Their efficacy in children for neuropathic pain is supported by case series (Nayak and Cunliffe, 2008). Systemic absorption of lidocaine is very low so side effects are minimal and therefore advantageous for children. Additional benefit comes from the patch providing a physical barrier to painful touch and a cool sensation from the patch itself. Cost can be prohibitive in some countries, and it is not licensed for use in many countries. Nortriptyline is similar to amitriptyline but is a secondary amine so exhibits fewer side effects. Alpha-2-delta ligands the alpha-2-delta (2-) ligands, sometimes referred to as gabapentinoids (gabapentin and pregabalin), are effective treatments in many forms of neuropathic pain (Backonja et al. There is evidence to suggest that these drugs selectively target those calcium channels that display abnormal activity (Li et al. Though it has been superseded by other anticonvulsants in the treatment of epilepsy, its use in paediatric neuropathic pain is now established. Gabapentin has also been successfully used in neurologically-impaired children with unexplained (neuro) irritability, improving behaviour and pain scores, which has contributed to the familiarity of the drug in paediatrics (Haney et al. There is less experience with pregabalin than gabapentin in the treatment of paediatric neuropathic pain. In adults, pregabalin has been licensed for generalized anxiety disorder, painful diabetic neuropathy, and been shown to be effective in fibromyalgia. The increased cost of pregabalin in some countries might make it prohibitive and favour gabapentin as a first-line treatment. Duloxetine has proven efficacy in painful diabetic polyneuropathy (Wernicke et al. Venlafaxine also has well-documented efficacy in painful diabetic polyneuropathy (Rowbotham et al. Duloxetine appears to be safe from an adverse cardiac conduction effect in adults (Wernicke et al. Its mechanism of action was originally thought to be due to depletion of substance P at peripheral nerve endings, though this does not fully explain its analgesic action. Low-concentration formulations of capsaicin are supported by modest evidence but require daily application which may limit its use in children (Derry et al. It should be considered as a second-line topical intervention in children with focal neuropathic pain where lidocaine patches are either unavailable or have failed to show improvement in symptoms after an adequate trial. Topical capsaicin is available in a variety of strengths and formulations to manage pain (Table 48. Although it is generally safe in terms of toxicity, the initial burning discomfort with application can result in problems with compliance, especially in children. These problems usually diminish with time, but the drug can take up to 4 weeks to produce benefit, requiring considerable patience in young patients. The newer stronger 8% capsaicin patch involves a single 60 min application with up to 12 weeks of effective subsequent analgesia. Opioids the term opioid refers to any compound synthetic or natural that activates the mu receptor; opiates specifically refer to drugs which derive directly from Papaver somniferum. Central inhibitory systems are the site of action of opioids which are agonists at inhibitory opioid receptors found in the brain, spinal cord, and periphery (see Hathway, Chapter 44, this volume); the action of endogenous opioid peptides is much less than that seen with opioid drugs. The historical dogmatic view that opioids do not demonstrate efficacy in neuropathic pain has long been refuted. Opioids have shown consistent analgesic efficacy in treatment of neuropathic pain (Eisenberg et al.
Zyprexa 10mg visa
Slifer medicine 5325 buy 5mg zyprexa visa, Adrianna Amari and Cynthia Maynard Ward Introduction Operant conditioning interventions for clinical pain involve the modification of environmental and social stimuli that are (1) antecedents (discriminative stimuli or setting events) to maladaptive pain behaviour or (2) consequent stimuli that maintain the maladaptive pain behaviour through positive reinforcement (social attention or assistance from others) or negative reinforcement (escape or avoidance of uncomfortable, effortful activity, or of social, academic, or work responsibilities). While aspects of operant conditioning theory have been included in the design of interventions to manage acute paediatric medical procedure-related pain (see Slifer et al. Before reviewing the history and empirical support for operant conditioning based interventions for pain, in general, and paediatric pain, in particular, it will be useful to note that much of the work in this area has been conducted by psychologists and behaviour analysts who have been trained in the research methods and conventions of the Experimental Analysis of Behaviour and Applied Behaviour Analysis (see Iversen, 2013; Cooper et al. These fields employ single-subject experimental designs in which each subject serves as his or her own control and careful, repeated observations are conducted on the same individual across time (referred to as a time series). The preference for single-subject methods and research designs arose from the philosophical perspective that information about what controls behaviour can be learned from studying its variability across environmental conditions within a single participant. Observations of the antecedents and consequences of target behaviour lead to hypotheses about controlling variables. Single-subject research involves systematic control and manipulation of antecedent or consequent variables in order to demonstrate and confirm the hypothesized functional control over the behaviour being studied. In this type of research, rather than obtaining a single or a few observations of a large sample of participants, the investigator obtains many observations of only one or a few participants. One important advantage of this type of research is that variability within subjects is considered important information to be studied rather than error variance to be controlled by averaging across a large group of subjects or by other statistical methods. In single-subject experimental design research an emphasis is placed on replication of demonstrated functional control both within a given subject on different occasions and across settings and replication of the same or similar results for a given intervention across repeated applications with a relatively small series of participants. This is particularly useful when developing and testing new intervention approaches based on cumulative individual subject evidence. This approach is also preferred by behaviour analysts because it allows for more individualization of intervention procedures while basing them on a consistent rationale and set of learning and conditioning principles. This is especially important for working with children whose behaviour patterns are developing based on their ongoing learning experiences. This individualized approach to intervention is a hallmark of Applied Behaviour Analysis, and it is especially useful for demonstrating the effectiveness of novel interventions. These interventions may later become the focus of more conventional randomized clinical trials that assess for generalizability of effects across larger samples of participants. In light of this research philosophy many of the studies discussed in this chapter employed single-subject experimental design and the strength of the evidence derives from replication across studies demonstrating the same or similar behavioural phenomena. This evidence base is supplemented by the few relevant group design studies and systematic reviews across studies that are available in the literature. That is, overt expressions or demonstrations of pain behaviour may frequently be followed by attention and attempts by family members and/or medical personnel to provide comfort (Fordyce et al. The patient in this case had complained of low back pain for 18 years and had decreased ability to function in the physical activities of daily living. She could maintain a maximum of 20 min of continuous activity without reclining to rest. When a pain episode occurred, she ceased all activity, laid down, took pain medication, and cried until the pain subsided. At these times she received a lot of solicitous and ministering attention from her husband and son. She had undergone surgical interventions to remove a herniated disk (the source of nerve root irritation) and a lumbosacral spine fusion to stabilize her spine. Therefore, the first intervention based on operant conditioning theory was to remove the contingent relationships between pain complaints and medication administration. Instead, whenever the patient was engaged in an out of bed activity and not speaking of her pain the staff provided positive social attention including praise for any observed increase in physical activity. In this way, pain behaviour was placed on operant extinction and physical functioning was differentially positively reinforced. Using these modified contingencies, a programme of occupational and physical therapy was developed that used rest and attention as the positive reinforcer for increasing participation in activities. As a result, the patient showed a marked increase in her activity level and her pain complaints nearly disappeared in a period of about 8 weeks. During the 1970s and 1980s, a few similar case studies of children were published using the same type of operant behavioural contingencies as those first described by Fordyce and colleagues (1968). For example, Sank and Biglan (1974) used operant procedures within a controlled case study to treat a 10-year-old boy with severe stomach pains. Miller and Kratochwill (1979) published another controlled case study in which time out was used to treat a 10-year-old girl with complaints of severe stomach pain that were hypothesized to be maintained by parental attention. The behavioural treatment in this case involved removing adult attention and social activities contingent on pain complaints. With this intervention, pain complaints in the home decreased from two per day during baseline observation to approximately one per week after treatment, and this improvement was maintained at 1-year follow-up. A similar decrease in conceptualization of pain behaviour in the adult clinical pain management literature. The operant conceptual framework for understanding chronic pain is that consequences that immediately follow pain behaviours may have a powerful influence on the probability of the pain behaviours occurring again in the future. According to Fordyce, the two general processes that are responsible for this operant conditioning are positive reinforcement and avoidance learning. Positive reinforcement suggests that the occurrence of pain behaviours will increase in frequency if followed by positive consequences. By definition, if a behaviour increases in frequency after a specific consequence consistently follows it, then whatever the consequence was is hypothesized to be a positive reinforcer. Avoidance learning of pain behaviour occurs when the frequency of a behaviour increases after that behaviour allowed the patient to escape or avoid aversive stimulation. In this process, pain behaviours such as limping, bracing, or activity avoidance become associated with decreased or no pain sensation, and as a result these behaviours are negatively reinforced and are maintained or increase in frequency. In chronic pain patients this process may become elaborated to the point that the anticipation of suffering becomes a conditioned aversive stimulus. Thus, in the context of anticipated pain, if the patient displays protective pain behaviours and pain perception or its exacerbation does not occur, then the same protective behaviours are more likely to be emitted in the future. Furthermore, Fordyce noted that once such avoidance learning occurs, it requires little ongoing reinforcement to maintain it. If a behaviour occurs due to anticipation of pain and motivation to avoid both the aversive experience of the anticipation (anxiety, physiological arousal) and the nociceptive stimulus, the patient will maintain the avoidance behaviour even if the nociceptive stimulation is never again experienced. In this situation the goal of operant treatment is to prompt and reinforce normative physical activity and arrange the environment such that the patient attempts typical physical activity without the self-protective pain behaviours, and does not experience pain or experiences it at much lower intensity or magnitude. These authors used a combination of multiple baseline and reversal single-subject experimental designs to document a reduction in the verbal and motor pain behaviour of a 3-year-old child across hospital bedroom, clinic, and physical therapy settings. Multiple behaviour change methods exist that can be focused on modifying pain behaviour directly, rather than attempting to directly change subjective pain perception. In that case the 21-year-old male with a 15-year history of pain, dizziness, and abnormal gait was treated with behavioural intervention because of his inactivity and severely impaired ability to walk. First, improved walking was established by reintroducing walking between parallel bars and positively reinforcing patient participation and achievement of increasing distances. After the provision of this multimodal intervention, the patient became normally active, ambulated normally, and returned to productive activity. After completing treatment he enrolled in and began attending college, and at 21 months post-treatment was maintaining his treatment gains. To demonstrate the effectiveness of this treatment, the authors employed a changing criterion single-subject experimental design. The role of aversive conditioning and escape-avoidance learning in the development and maintenance of chronic pain behaviour As already discussed, early operant conceptualizations by Fordyce and colleagues focused primarily on operant extinction of positively reinforced pain behaviour (eliminating pain behaviour-contingent positive reinforcement). However, these investigators subsequently conceptualized some pain behaviour in terms of escape-avoidance learning. For example when pain behaviour occurs in the context of physical exertion, the patient will discontinue the exertion and thereby escape the pain associated with the exertion. With experience, the patient may learn not only to stop physical activity that produces pain or discomfort, but may also learn to avoid the situations in which physical activity might be required. Thus, an adult may begin to avoid going to work, leaving the house or even getting out of bed. Children and adolescents may learn to avoid going to school, participating in athletics, or even having social interactions with peers. This publication described a procedural innovation specifically designed to modify chronic pain behaviours that were hypothesized to have been acquired through avoidance learning.
Cheap zyprexa amex
This strategy was evaluated in an interesting study (0) that evaluated patients who showed poor responses to 2 weeks of treatment with risperidone symptoms ms women discount zyprexa 20 mg without a prescription. Subjects were then randomized to either staying on risperidone or changing to olanzapine. There was a very small, but statistically significant, advantage for subjects who were changed to olanzapine. The results provide some useful guidance for clinicians in that changing antipsychotics may be somewhat helpful in the absence of a response. However, patients who are poor responders to an adequate trial of an antipsychotic (other than clozapine) are seldom vigorous responders to other antipsychotics. Clozapine for Poor Responders Patients who respond poorly to first- and second-generation antipsychotics may improve if they are treated with clozapine. This was first demonstrated in a large multicenter trial (2) that carefully characterized patients as treatment refractory (or poor responders) by reviewing their clinical history and by treating them prospectively with haloperidol. When compared with chlorpromazine, clozapine was superior for a broad range of psychopathology, including positive and negative symptoms, as well as anxiety and depression. The results from this study led to the approval of clozapine in the United States for individuals with treatment-refractory schizophrenia. The advantages for clozapine in this population have been reinforced by other trials comparing clozapine to both first- and second-generation antipsychotics. A large study found an advantage of clozapine over olanzapine for schizophrenia patients with suicidal ideation or suicidal behaviors. Other studies (3) suggest that clozapine has advantages for hostility and aggression in treatment-resistant schizophrenia patients. Clozapine for Partial Responders There is also evidence that clozapine can be helpful for schizophrenia patients who are stable, but are burdened by psychotic symptoms. In that study, subjects who were discontinued from their antipsychotic for a lack of efficacy during Phase were randomly assigned to either clozapine or another second-generation agent (5). In a study from the United Kingdom (6) patients who were partial responders to antipsychotics were randomized to either clozapine or an antipsychotic selected by their clinician. Taken together, these studies indicate that patients who are burdened by disturbing psychotic symptoms should receive a clozapine trial. However, patients who are functioning relatively well in the community may derive substantial benefits if symptoms such as hallucinations or suspiciousness can be reduced. In addition, clinicians who are allowing patients to experience psychotic symptoms for months or even years before treating them with clozapine may be waiting too long. As noted earlier, poor or partial responders can usually be identified after just a few weeks. Schizophrenia 24 Starting Patients on Clozapine Prior to starting clozapine, the clinician should assure that there is a system in place for blood monitoring. If clozapine is well tolerated, the dose can be increased by 25 mg every other day until a dose of 300 to 450 mg daily is reached. If patients are hospitalized, the titration can be more rapid, with dosage increases of 25 mg daily. In most cases, patients should be dosed two or three times daily, with the larger dose administered before bedtime. In nearly all cases, patients will be changing from another antipsychotic to clozapine. The other antipsychotic should be continued until the patient reaches a dose of clozapine that may have therapeutic activity. As patients reach this clozapine dose, the other antipsychotic should be gradually decreased and eventually discontinued. Patients should receive clozapine for at least 3 months to determine if this is an effective drug. A number of studies indicate that patients are more likely to respond when their clozapine plasma levels are greater than 350 ng/ml (7). If the laboratory reports concentrations as clozapine plus norclozapine, levels will be higher. There is no evidence that higher levels than 350 ng/ml are associated with increased effectiveness. A reasonable strategy is for clinicians to monitor plasma concentrations when patients are not showing an adequate response or when side effects are limiting the dose. In addition to sedation and hypotension, common side effects are anticholinergic side effects including constipation, difficulty urinating, and blurry vision, low grade fevers, constipation, gastrointestinal discomfort, tachycardia, and sialorrhea. Since constipation can become severe, patients should be warned to increase their fluid intake and to use stool softeners or other treatments at the earliest signs of discomfort. Patients should also be warned about more serious side effects that can occur early in treatment. Seizures are relatively common during the first weeks of clozapine treatment, and are more common when patients are receiving higher doses. Patients should probably be warned not to drive during the first weeks of clozapine treatment. In the great majority of cases, seizures can be managed by reducing the dose or adding an anticonvulsant such as valproate. Since clozapine can also be associated with metabolic effects, including weight gain, elevated lipids, and insulin resistance, patients should be told to monitor their weight, and clinicians should monitor lipids and blood glucose. In the great majority of cases, myocarditis occurs during the first 2 months of clozapine treatment. Early symptoms may include fever (48%), dyspnea (35%), "flu-like illness" (30%), chest pain (22%), and fatigue (7%) (8). The problem is that some of these symptoms are relatively common during the early weeks of clozapine treatment, and they also raise concerns about agranulocytosis. If there is any suspicion of myocarditis, plasma troponin (9) and c-reactive protein (20) levels should be ordered and a cardiologist should be contacted. Monitoring for Agranulocytosis Patients receiving clozapine need to be monitored for evidence that they have or will develop agranulocytosis. The question that torments many clinicians is when to discontinue clozapine when patients develop neutropenia or when the neutrophil count is dropping. If rechallenged monitor weekly for year before returning to the usual monitoring schedule. As a result, clozapine treatment can be particularly challenging with occasional interruptions. Managing Partial Responders to Clozapine It is not uncommon for patients to improve on clozapine, but nevertheless continue to experience psychotic symptoms. A number of studies have explored adding a low dose of a high-potency antipsychotic. A meta-analysis of studies that added a second antipsychotic to clozapine (2) found that open label studies tended to favor adding a second antipsychotic, but double-blind studies did not find statistically significant effects. As a result, this may be a useful intervention when patients continue to experience disturbing symptoms on clozapine. Studies in this area include mostly case reports that tend to be biased in favor of positive reports. Although most well-controlled studies have found positive results, the effect sizes have varied. Prevalence of and risk factors for medication nonadherence in patients with schizophrenia: a comprehensive review of recent literature. Validity of electronically monitored medication adherence and conventional adherence measures in schizophrenia. Effect of cannabis use on the course of schizophrenia in male patients: a prospective cohort study. The effect of cannabis use and cognitive reserve on age at onset and psychosis outcomes in first-episode schizophrenia. Time course of improvement with antipsychotic medication in treatment-resistant schizophrenia. Early response to antipsychotic drug therapy as a clinical marker of subsequent response in the treatment of schizophrenia. Clozapine for the treatment-resistant schizophrenic: a double-blind comparison versus chlorpromazine/benztropine.
Discount zyprexa 2.5 mg free shipping
The majority of studies used 15 to 30 min and had positive results medicine 223 quality 20 mg zyprexa, and as little as 10 min seems to be effective. In the situations where it is impossible to hold the infant, alternative strategies emphasising maternal presence such as olfactory or auditory stimuli, or facilitated tucking may be used as adjuvant therapy in conjunction with sweet taste or in combination as more holistic sensorial saturation. Further studies are required to determine the efficacy of these strategies for repeated procedures over time. We know that the uptake of any clinical practice change generally lags behind dissemination of the research findings (Graham et al. Using mothers and families as providers of comfort presents several additional several challenges, requiring a paradigm shift. Health care providers will need to further relinquish their traditional care model to consider parents as partners in provision of care rather than bystanders; thus placing increased emphasis and time for the coordination of care, scheduling, and timing of procedures to enhance parental involvement. The skill of the health care providers conducting the procedure also needs to be considered in relation to feasibility. Issues regarding safety and ergonomic needs of the care providers have also been reported (Campbell-Yeo et al. Conclusion Mothers have a unique relationship with their infant and a special role in comforting their infant in the face of pain. Data exist to support that mothers are better than others at comforting their infant, either through some biological mechanism or because of the profound caring they have for their infant, normally stronger than others. Given their effectiveness, it is highly recommended that mothers be included in comforting their infant during painful procedures whenever possible. The oxytocin antagonist 1-deamino-2-D-Tyr-(Oet)-4-Thr-8-Orn-oxytocin reverses the increase in the withdrawal response latency to thermal, but not mechanical nociceptive stimuli following oxytocin administration or massage-like stroking in rats. Object relations, dependency, and attachment: a theoretical review of the infant-mother relationship. The effect of kangaroo care on pain in premature infants during invasive procedures. Promoting shorter duration of ventilator treatment decreases the number of painful procedures in preterm infants. Case example Madeline is a 7-day-old preterm neonate who was delivered 11 weeks early at 29 weeks gestational age. For example, heel lance for blood collection, the most common, occurs one to two times a day. Madeline becomes very distressed during the heel lance as exhibited by her facial actions and changes in her physiological stability. Oral glucose and parental holding preferable to opioid in pain management in preterm infants. Effect of multisensory stimulation on analgesia in term neonates: a randomized controlled trial. Sensorial saturation: an effective analgesic tool for heel-prick in preterm infants: a prospective randomized trial. Comparison of sucrose, expressed breast milk, and breast-feeding on the neonatal response to heel prick. Effects of colostrum in newborn humans: dissociation between analgesic and cardiac effects. The impact of adult behaviors and vocalizations on infant distress during immunizations. Procedural pain management for neonates using nonpharmacological strategies: part 2: mother-driven interventions. A comparison of nurse and mother attitudes regarding maternal skinto-skin care as a pain relieving strategy during heel stick for preterm neonates. A comparison of nurse and mother attitudes regarding maternal skinto-skin care as a pain relieving strategy during heel lance for preterm neonates. Cobedding and recovery time after heel lance in preterm twins: results of a randomized trial. Rey-Martinez Kangaroo Mother Program: an alternative way of caring for low birth weight infants Skin-to-skin contact and/or oral 25% dextrose for procedural pain relief for term newborn infants. Breastfeeding or oral sucrose solution in term neonates receiving heel lance: a randomized, controlled trial. Kangaroo Care modifies preterm infant heart rate variability in response to heel stick pain: pilot study. Randomized crossover trial of kangaroo care to reduce biobehavioral pain responses in preterm infants: a pilot study. Facilitated tucking: a nonpharmacologic comfort measure for pain in preterm neonates. The use of breast-feeding for pain relief during neonatal immunization injections. Neurobehavioural assessment of skin-to-skin effects on reaction to pain in preterm infants: a randomized, controlled within-subject trial. Evaluation of analgesic effect of skin-to-skin contact compared to oral glucose in preterm neonates. Parental role alterations experienced by mothers of children with a lifethreatening chronic illness In S. Use of facilitated tucking for nonpharmacological pain management in preterm infants: a systematic review. The relationship between caregiver sensitivity and infant pain behaviors across the first year of life. The effect of Kangaroo Care on physiologic responses to pain of an intramuscular injection in neonates. Olfactory function in the human fetus: evidence from selective neonatal responsiveness to the odor of amniotic fluid. Breastfeeding or breastmilk to alleviate procedural pain in neonates: a systematic review. Comparison of infant preferences and responses to auditory stimuli: music, mother, and other female voices. Alternative female kangaroo care for procedural pain in preterm neonates: a pilot study. Paternal vs maternal kangaroo care for procedural pain in preterm neonates: a randomized crossover trial. Enhanced kangaroo mother care for heel lance in preterm neonates: a crossover trial. Kangaroo mother care diminishes pain from heel lance in very preterm neonates: a crossover trial. The effect of Kangaroo Care on behavioral responses to pain of an intramuscular injection in neonates. Kangaroo Care (skin contact) reduces crying response to pain in preterm neonates: pilot results. Behavioral and adrenocortical responses to stress in neonates and the stabilizing effects of maternal heartbeat on them. Non-nutritive sucking and facilitated tucking relieve preterm infant pain during heel-stick procedures: a prospective, randomised controlled crossover trial. Neurophysiologic assessment of neonatal sleep organization: preliminary results of a randomized, controlled trial of skin contact with preterm infants. Intraventricular somatostatin-14, arginine vasopressin, and oxytocin: analgesic effect in a patient with intractable cancer pain. Human newborns prefer human milk: conspecific milk odor is attractive without postnatal exposure. Analgesic effect of expressed breast milk in procedural pain in term neonates: a randomized, placebo-controlled, double-blind trial. The efficacy of facilitated tucking for relieving procedural pain of endotracheal suctioning in very low birthweight infants. Intrathecal administration of oxytocin induces analgesia in low back pain involving the endogenous opiate peptide system. Weydert Summary Because of the interest of patients and physicians, there has been increasing research into the use of botanical agents, nutritional supplements, and diet as a means to manage pain.